Aloft Integrated Wellness
Pediatric Practice Bridges the Gap Between Mental and Physical Health Using Collaborative Care with Mirah
Aloft Integrated Wellness
When Jessica Lyons approached Ben Hillyard in 2019 with the idea to build their own mental health practice, Ben agreed under the condition they build something different. He wanted to explore uncharted territory to truly change the lives of children and their caregivers.
And so began Aloft Integrated Wellness (“Aloft”), a mental health practice specializing in pediatric populations. Together, Ben, Jessica, and their team of providers are working to bridge the gap between pediatric mental and physical health care.
Collaborative Care: Aloft’s Way
Shortly after launching in 2019, Aloft partnered with Exeter Hospital’s Core Pediatric and Adolescent Medicine to embed a behavioral health team within primary medical care. The purpose of this partnership was to leverage Collaborative Care (CoCM), an integrated care strategy that combines the efforts of complementary healthcare professionals to treat mental health conditions that may have otherwise slipped through the cracks in a primary care setting. CoCM is a data-driven and evidence-based approach that enables the care team to routinely monitor patient outcomes using measurement-based care (MBC).
The team at Aloft took this a step further by pioneering their own take on this innovative model to work with pediatric populations. Their approach could not be more timely as the American Academy of Pediatrics, American Academy of Child and Adolescent Psychiatry, and Children’s Hospital Association have declared a State of Emergency for Youth Mental Health and the U.S. Surgeon General issued a youth mental health advisory.
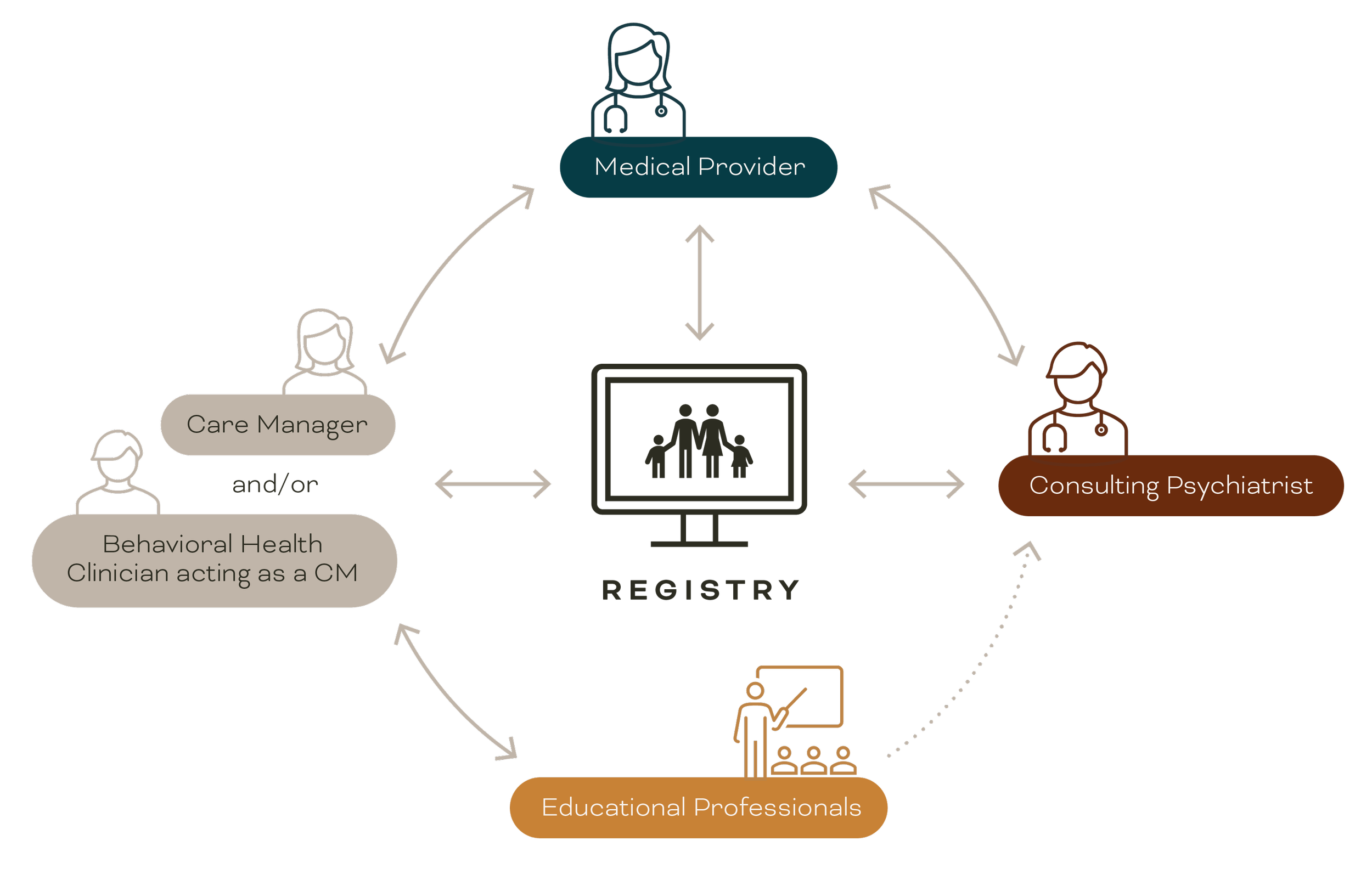
Patients are referred to Aloft’s program by their Primary Care Provider (PCP) based on behavioral health concerns. Once enrolled in the program, patients are introduced to a Behavioral Health Clinician (BHC) and/or a Care Manager (CM). Together, the BHC and/or CM act as the hub of communication between the patient/caregivers and their network of providers. The BHC and/or CM meet regularly with the PCP and a Consulting Psychiatrist to review the program’s patient caseload and adjust prescriptions and treatment plans according to patient outcomes. Patients remain in the program for roughly six months, after which they are discharged or enrolled in longer-term programs, depending on clinical needs.
Aloft’s program also addresses the educational system challenges around mental health for students. As the system currently stands, insufficient communication between schools and healthcare providers is common despite the wealth of information that could lead to more effective interventions. This disconnect often results in barriers to care. Using tools designed to address this very issue and placing emphasis on collaborative dialogue with schools, the Aloft model brings important educational data into medical decision-making and progress monitoring.
“The fact that Mirah allows for multiple respondents helps our team gather clinical information from a systems perspective. We receive feedback from parents, teachers, and patients in a way that creates a more full picture.”
Jessica Lyons
Using Mirah to Drive Collaborative Care
To enable their innovative model, Aloft partnered with Mirah, the industry’s leading measurement-based care solution. The Mirah platform streamlined measurement of patient outcomes and assisted caseload management by acting as a patient population registry.
Mirah automatically sends mental health assessments, also called measures, on a regular basis according to each individual patient’s treatment plan. Measures can also be sent to a patient’s parents/caregivers or related educational professionals as needed. Mirah’s library of over 400 clinically validated assessments includes some of the most common and well-known measures such as the PHQ-9 and GAD-7, which screen for depression and anxiety. However, the robust library also contains an array of measures across a wide spectrum of conditions such as ADHD, trauma, and eating disorders. This is a game changer for Aloft when it comes to screening, treating conditions, and customizing care for their patients.
“All the other available products out there are basically dedicated to the PHQ-9 and the GAD-7… When we are presented with a problem, there can be so many integrated or connected issues. Using Mirah for measurement-based care allows us to investigate further, take a wider view, or pivot when a patient isn’t improving. Our model highlights the powerful impact data has on treatment.”
- Ben Hillyard
As patients complete measures, the Mirah platform collects and synthesizes those responses to Aloft’s care team, who then review the data against the patient’s individual target outcome and discuss any trends or necessary changes in treatment.
By using Mirah as a patient population registry, Aloft can collectively track clinical outcomes and patient engagement across their defined caseload. This approach enables efficient and responsive psychiatric caseload review. Aloft’s BHC and CM meet weekly with the Consulting Psychiatrist. In these meetings, the providers review each patient and their measured outcomes, prioritizing those who are not improving as expected and may require treatment adjustments.
“We also take kids off medication as much as we put kids on it, which has been amazing to us. One of the things that we pride ourselves on is our ability to quickly change course if the medication isn't effective. If it's not working, let's try something else.” - Ben Hillyard
“This model alleviates access - which saves lives, decreases stigma, and increases whole child view.”
Denise Toshach, MD - Core Physicians
The Results
Aloft is the first pediatric practice in the state of New Hampshire to successfully implement and bill for CoCM, and the response has been overwhelmingly positive. The program has seen many new patients transfer into its primary care location based on word-of-mouth between parents alone.
By installing the Care Manager as the “core communicator,” Aloft alleviates the stress of many parents and caregivers. By surrounding the primary care team with behavioral health supports including the consulting psychiatrist, this model treats the whole person.
When asked about the program’s key successes, Hillyard responded:
“When the parents start crying, ‘thank you,’ that's really it. And that's been common, because parents become overwhelmed. They have to run between the primary care doctor, the therapist, the OT, the school, and the special ed team. Without our model, no one holds the full picture. Parents are the translators of all those different dialects and terminology between places to pass along the recommendations to the next provider. We simplify that for them which leads to better care and better outcomes.”
In describing visions for the future of Aloft, Hillyard shared: “Our goal is to change pediatric mental health across the country. And that's no joke. The system is broken and we’re fixing it.”
The Aloft model has gained national attention in a short period of time, including a case study published in SG2 and nomination for the 2023 Small Business Association National Business of the Year award. The team remains focused on their goal of changing pediatric mental health across the nation – consulting with other healthcare systems to implement their data-driven, innovative model using measurement-based care.